Introduction:
TCR αβ+/CD19+ depletion in hematopoietic stem cell transplantation (HSCT) is an emerging graft manipulation technique to help overcome the HLA barrier in the mismatched or haploidentical transplant setting and reduce or prevent graft-versus-host disease. Limited research has explored the impact of various donor sources, and type of malignancy on the outcomes of TCR αβ+/CD19+ depleted HSCT for acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), and myelodysplastic syndrome (MDS). Therefore, we performed a comprehensive meta-analysis of published clinical studies using individual patient data (IPD) to address this scientific gap.
Methods:
This meta-analysis combined patient-level data from studies involving AML/MDS and ALL patients treated with TCR αβ+/CD19+ depleted HSCT. By utilizing the IPDfromKM technique, we reconstructed time-to-event data from aggregated Kaplan-Meier curves, specifically focusing on overall survival (OS), disease-free survival (DFS), and GVHD-free, relapse-free survival (GRFS). Additionally, we conducted parallel meta-analyses to calculate the pooled incidences of GVHD, graft failure, mortality, as well as CMV and EBV reactivation, and sinusoidal obstruction syndrome (SOS) using aggregate data. All analyses were performed using STATA software. Our comprehensive literature search included publications up to May 2023, excluding studies with significant sample overlap.
Results:
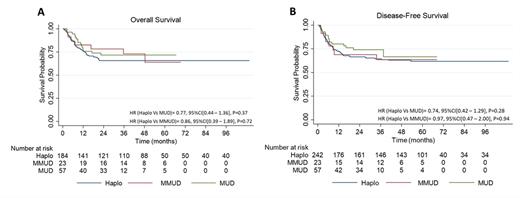
The meta-analysis incorporated 817 children with AML/MDS or ALL from 12 studies. Successful primary engraftment was observed in 95% of patients (95% CI: 92 - 98), with an average time to neutrophil and platelet engraftment of 12 days. The incidence of acute GVHD grades I-II was 24% (95% CI: 14 - 34), while grades III and IV were 11% (95% CI: 3.0 - 0.18). Chronic GVHD was observed in 19% of patients (95% CI: 11 - 28). The relapse and graft failure rates were 25% (95% CI: 19 - 32) and 6% (95% CI: 2.0 - 9.0), respectively. The all-cause mortality was 34% (95% CI: 29 - 38), with HSCT-related mortality at 11% (95% CI: 8.0 - 13), while relapse-related mortality accounted for 22% (95% CI: 17 - 28). At a median follow-up of 2.55 years, the 1-year and 5-year OS rates were 74.7% (95% CI: 60.6 - 78.3) and 64.4% (95% CI: 59.9 - 68.5), respectively. No significant differences in OS were found between ALL and AML/MDS patients (HR= 0.99, 95% CI: 0.48 - 2.02, P=0.98) or between different donor types (Figure 1A). The DFS rates at 1- and 5-year were 72.8% (95%CI: 67.6 - 77.3) and 61.8% (95%CI: 56.1 - 67.0), respectively. No significant differences in DFS were observed between ALL and AML/MDS patients (HR = 0.74 95%CI: 0.48 - 1.14, P=0.17) or between different donor types (Figure 1B). The overall 1- and 5-year GRFS rates were 71.1% (95% CI: 64.1 - 77.4) and 63.0% (95% CI: 55.3 - 69.8), respectively. The overall incidence of CMV and EBV reactivation was 33% (95% CI: 19 - 46) and 16% (95% CI: 0 - 38), respectively.
Conclusions:
Our meta-analysis confirms the effectiveness and safety of TCRαβ and CD19-depleted HSCT for hematological malignancies, demonstrating high engraftment success, low graft failure, and a manageable incidence of acute and chronic GVHD. The consistently favorable outcome data across different donor types and malignancies support the broad applicability of this form of graft manipulation.
Disclosures
Otto:Cellectar Biosciences: Consultancy; yMabs Therapeutics: Consultancy.